What are Health Inequalities?
Health Inequalities are the unfair and avoidable differences in the health of people in our society.
Health inequalities is a term used by researchers and policy makers to refer to the unfair nature of health differences between social groups, brought about by the conditions they are born and live in. They are avoidable as these differences do not happen randomly but rather are determined by social factors largely out of an individual’s control.
The most recent statistics for Northern Ireland show big, regional health inequalities. Watch this video to find out more.
What causes them?
Health Inequalities are the result of imbalances of power, wealth and resources. The unequal distribution of power, wealth and resources is sometimes called the fundamental causes of health inequalities. They are fundamental because they are the basis from which health inequality is formed.
The fundamental causes influence the distribution of wider environmental influences on health and access to services and wider society. This in turn shapes people's individual experiences and results in health inequalities.
Social Determinants of Health
Health is known to be affected by a broad range of factors. These include living and working conditions; community and family networks; social and economic conditions; and environmental factors. These non-medical factors are called the Social Determinants of Health (SDOH). These SDOH are influenced at local, national, and international level and clearly go beyond the ability of any individual to control. The evidence is clear and growing. Issues such as stress, social isolation and a lack of control can all impact on a person’s health. When it comes to health inequalities, nothing can be looked at in isolation. The root causes are both interconnected and accumulative.
Interconnected: Living and working conditions are influenced by education and community networks. These, in turn, are influenced by family income and neighbourhood. If a person experiences one inequality, then they are at greater risk of experiencing others.
Accumulative: The longer people live in stressful situations where they feel out of control, the greater the toll on health is likely to be.
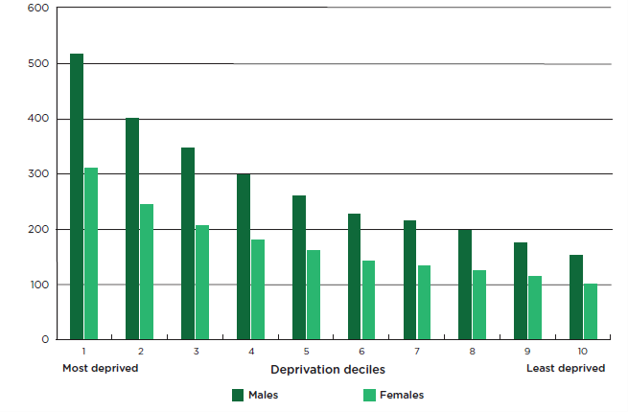
Income Inequality/Social Gradient
Variations in health status generally follow a gradient, with overall health tending to improve with improvements in socio-economic position. Therefore, people with a higher income generally enjoy better health and longer lives than people with a lower income. The rich are healthier than the middle classes, who, in turn, are healthier than the poor. This is known as ‘the social gradient’ – every step up the socio-economic ladder leads to an improvement in health outcomes. The social gradient in health means that health inequalities affect everyone.
(Source: Marmot, M, Allen J. et al. (2020). Health equity in England: The Marmot review 10 years on. London: Institute of Health Equity.)
Poverty
Since the Black Report (1980) made the link between socio-economic status and health, there has been a growing body of evidence that disadvantage, which accumulates throughout a person’s life, has a negative impact on their health. Poverty is intricately linked to people’s access to resources and services. For example, research shows clear links between a cold house and lower educational attainment. With higher numbers of absences, children living in poverty are less likely to achieve their academic potential and become isolated from peers due to lower participation in school life. In such ways, poverty places barriers on people to fully accessing services that the more affluent can access with ease.
In work poverty
A worrying trend is the increase in workers living in poverty. Research from the Living Wage Foundation discovered that 21% of workers in Northern Ireland are paid below the real living wage. The old mantra of ‘work your way out of poverty’ is clearly untrue today. The rise in uncertain and temporary work has left many trapped in a cycle of insecure employment. Zero-hour contracts, the gig economy and a rising cost of living, all contribute to a situation of the ‘working poor’.
Proportionate Universalism
Proportionate universalism is the resourcing and delivering of universal services at a scale and intensity proportionate to the degree of need. Services are therefore universally available, not only for the most disadvantaged, and are able to respond to the level of presenting need. Proportionate universalism is a strategy of support that can address burden of disease across a number of determinants of health to narrow the gap in health inequality.
Reducing Health Inequalities
WHO Commission on SDOH - three principles of action
1) Improve the conditions of daily life – the circumstances in which people are born, grow, live, work and age.
2) Tackle the inequitable distribution of power, money, and resources – the structural drivers of those conditions of daily life – globally, nationally, and locally.
3) Measure the problem, evaluate action, expand the knowledge base, develop a workforce that is trained in the social determinants of health, and raise public awareness about the social determinants of health.
What CDHN is doing...
We believe in the power of people and communities to identify and solve local issues. As an organisation, we are committed to building power with the collective to redress power imbalances and ensure that people are more involved in the decisions that affect their lives. You can read more about community development here.
All of our work has a focus on reducing health inequalities. We believe that this will only be achieved when communities are at the heart of decision-making processes. Through our work, communities and decision makers are supported to recognise and utilise assets, to work together to develop solutions, take action to improve lives and create a fairer, more equal society.
Projects
Building the Community-Pharmacy Partnership (BCPP) supports communities and community pharmacists to work in partnership to address locally defined needs so that people make connections, listen to and understand each other better and work together to address the social determinants of health and health inequalities.
Elevate is a programme of support for the community, voluntary and public sectors. It provides opportunities for the development of skills, knowledge and expertise in community development as a way to tackle health inequalities.
Policy
CDHN works to strengthen the understanding of decision makers, practitioners and communities as to how social policies and programmes interact with social determinants of health and influence health inequalities. This is achieved through the provision of information, workshops, advocacy and policy responses.
Resources
We offer some useful resources through the Elevate programme to help you better understand and engage with health inequalities and community development. We are continually updating this section with useful websites, links and videos - please have a look!
Take Action
Sign up for some Elevate training


